About cervical cancer and its causes
What is cervical cancer?
Cancer of the cervix occurs when some cells in the cervix change and grow abnormally. These cells can also spread to other parts of the body.
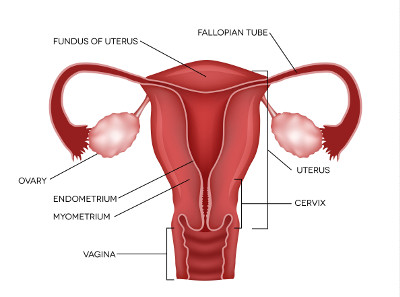
The cervix is the area between the vagina and uterus (womb).
What causes cervical cancer?
The human papillomavirus (HPV) causes over 90% of cervical cancer.
What is HPV?
HPV is a common virus that is spread by genital skin-to-skin contact during sexual activity. It is so common that many people have it at some point in their lives and never know it as there are usually no symptoms.
The body normally clears the virus in 1-2 years.
When the virus persists for 10 or more years, it may cause abnormal changes to cells of the cervix. Left untreated, these changes can develop into cervical cancer.
Different types of HPV
There are over 100 types of HPV, only a small number of these types (also called 'strains') can cause cervical cancer. These types are also called high-risk HPV (hrHPV).
The most common types of HPV that cause cervical cancer are types 16 and 18. There are 12 other cancer causing HPV types. These cancer causing HPV types are also called oncogenic HPV. They can also cause cancers in other parts of the body in both men and women.
HPV vaccine
The HPV vaccine works best if you have it before you are sexually active and exposed to the HPV virus. If you have already been exposed to HPV, the vaccine will be less effective.
The HPV vaccine protects against HPV types that can cause several cancers including cervical, vaginal, vulval, anal, throat, and penile. The vaccine also protects against genital warts.
From 2018, Gardasil®9 replaced the previous HPV vaccine (Gardasil®) provided for free through the National Immunisation Program (NIP). Gardasil®9 protects against nine types of HPV, seven of which can cause cancer and two that cause genital warts.
The NIP provides the Gardasil®9 vaccine to school aged children, typically at 12 to 13 years old.
Regular cervical screening is still recommended even after having the vaccine as the vaccine does not cover all types of HPV.
About the HPV vaccine?
The best time to be immunised against HPV is before you become sexually active. People who have had sexual contact may have already been infected with some types of HPV. If you have already been infected with any of the HPV types included in the HPV vaccine, the vaccine will not protect you against cancers caused by those HPV types. But you will be protected against the other HPV types contained in the vaccine.
People under 26 years old can get the HPV vaccine free from a GP, council immunisation clinic or pharmacist immuniser under the National Immunisation Program (NIP), if they did not receive the vaccines at school. This is called catch-up vaccination.
If you are 26 years or older, you can still have the vaccine through your GP. There is a cost for this vaccine. Ask your GP for further information.
Vaccination History
You can check your vaccination history at Australian Immunisation Register (AIR).
What is the HPV school vaccination program?
The HPV vaccine is available for free to young Australians through the NIP.
The school-based vaccination program was introduced in 2007, and provides the vaccine to children aged approximately 12 and 13 years. If the vaccine is missed at school, GPs, council immunisation clinics or pharmacist immunisers also offer the vaccine as part of a catch-up program for young people under the age of 26 years.
How many doses of the HPV vaccine are needed?
Only one dose of HPV vaccine is needed for full protection if the dose is given before the age of 26.
Those aged 26 years and over require three doses.
