Care@home
A translator or interpreter in your preferred language is available when you phone Care@home on 1800 973 363.
Care@home is not an emergency or urgent care service.
Care@home assesses, monitors and supports eligible people to safely recover from illness at home. People who are very ill should seek urgent care from their GP, healthcare provider, hospital emergency department or by phoning Triple Zero (000).
Care@home
Care@home is a state-wide interdisciplinary service that remotely supports patients, to better self-manage their illnesses and chronic conditions in their own home using virtual care technologies, improving patient health outcomes and reducing potentially preventable hospital admissions.
This virtual care service aims to provide a single point of access for home and community-based care; making it easier for both consumers and clinicians to identify what care pathways are available to support people in their preferred environment.
View the Model of Care for Care@home here.
Care@home has three service arms:
Acute Virtual Monitoring Program (AVMP):
- This program offers short-term care at home for people with acute illnesses like respiratory infections (Covid, flu, croup, RSV), cellulitis, gastroenteritis, UTIs, and flare-ups of chronic conditions such as COPD, asthma, heart failure, and diabetes. Some other conditions may be considered case by case. Patients are enrolled for 7 to 10 days, with 24/7 nursing support and access to doctors from 9 AM to 9 PM, seven days a week.
Chronic Disease Management Program (CDMP):
- This virtual program helps people with long-term conditions stay healthier and avoid hospital visits. It offers health coaching, education, and care coordination to support better self-management. Patients work with the Care@Home team to set and achieve health goals while being connected to the right healthcare services for their needs.
GP Now
- A team of General Practitioners who deliver virtual clinical consultations, support for GP Registrars and junior doctors and short-term primary care deployment to community settings where there are critical risks to the delivery of services.
How to enrol
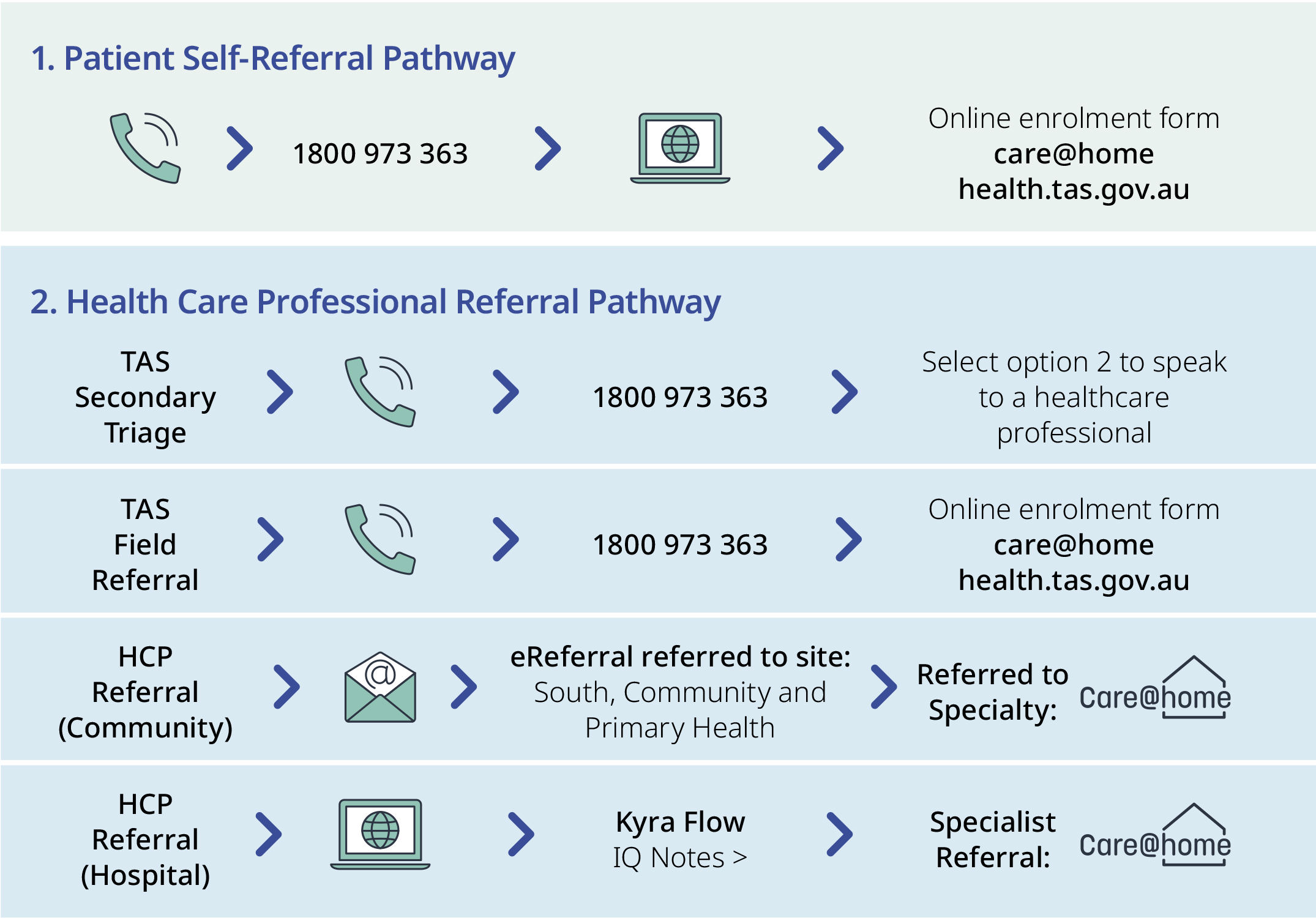
Care@home offers two referral pathways: Patient Self-Referral and Health Care Professional Referral.
For the Acute Virtual Monitoring Program self-referrals are only accepted for those with acute respiratory illness. All other referrals must be completed by a healthcare professional.
For the Chronic Disease Monitoring Program, referrals can be either by self-referral or healthcare professionals.
Once the referral has been received, an initial clinical assessment will occur within 2 - 24 hours of self-enrolment or health professional referral depending on the source of referral and service being requested.
Please note – Care@home is not an emergency or urgent care service, if your patient requires emergency care, please call 000.
For Acute Respiratory Illness Self Referral
If you test positive to COVID-19, flu, respiratory syncytial virus (RSV), or other flu-like illness on a PCR test:
- Complete an online enrolment form to enrol in Care@home.
You must complete this form to enrol in Care@home.
If you test positive to COVID-19 or other respiratory illness on a rapid antigen test (RAT):
- Complete an online enrolment form to enrol in Care@home.
- You no longer need to register a positive RAT test in Tasmania.
If you cannot complete an online enrolment form, call the Care@home team on 1800 973 363
If you enrol, the Care@home team will assess your situation and needs to determine the level of care you require. Your level of care will be influenced by risk factors such as:
- your age
- vaccination status
- symptom severity
- if you have a suppressed immune system
- if you are pregnant
- if you identify as Aboriginal and/or Torres Strait Islander.
Your Care@home care team
While you are enrolled in Care@home you will be supported by staff from the Department of Health including nurses, doctors, allied health professionals and our admin team.
Our admin team are the first people you will speak with. They will confirm your details and enrol you in the Care@home system.
If you require clinical advice, the admin team will organise for a nurse or doctor to contact you as soon as possible.
With your consent, your existing healthcare provider, such as a general practitioner (GP), will be consulted to make sure we provide you with the most suitable support and for discharge information/support when you leave Care@home.
Virtual healthcare monitoring kit
If you are given a Care@home virtual healthcare monitoring kit, the Care@home team will let you know how your kit will be provided to you. The kit includes a monitor to check your oxygen levels and heart rate, a thermometer to check your temperature, and a smartphone device with MyCareManager application for the team to monitor your results virtually.
You will submit checks at least daily using the smartphone. The information will feed directly back to the Care@home clinical team, who will contact you if required and make sure you have the care you need.
When you leave the program, the Care@home team will contact you to arrange the return of the virtual healthcare monitoring kit.
You may be able to utilise a virtual appointment through MS Apps. More information is available here.
When to contact Care@home
Even if you’re feeling well or only slightly unwell, it’s important to watch your symptoms and understand when you might need to get more help. For help with this, please visit the health direct website and complete the symptom checker.
If you feel that your symptoms are getting worse, phone the Care@home team on 1800 973 363 for advice. If you are very unwell, you may be transferred to hospital.
When to call an ambulance
You should always call an ambulance if:
- you are experiencing severe symptoms, like shortness of breath or difficulty breathing
- you think it’s an emergency
- you think your life or someone else’s life is in danger.
Call Triple Zero (000) for an ambulance. You should tell the operator if you have COVID-19.
Social and welfare support
You can contact the Care@home team on 1800 973 363 to access support for any other health or social needs.
GPs and other community partners like your local pharmacy are available to provide extra support.
GP NOW
How to contact the team
The GP NOW Rapid Response team can be contacted through the Care@home team on 1800 973 363 or [email protected]
What is the GP NOW Rapid Response service?
The GP NOW Rapid Response service is being developed to provide crisis support and intervention to communities where private general practice has experienced challenges. This includes where there are sudden or unplanned practice closures.
Provides General Practitioners who deliver clinical consultations as well as support for GP Registrars and junior doctors with supervision and training needs. Offering both virtual care support and short-term primary care deployment to community settings for at risk primary care services.
Five GPs were appointed to join the GP NOW Rapid Response service in October 2024 and will be based around the state.
The team is integrated into Care@home to support the Care@home team as and when required.
What role will the service fulfil?
- Improved outcomes and access to health care for our community
- Enhanced support for General Practice where there is critical risk to service continuity.
- Provide interim supervision to GP Registrars, International Medical Graduates (IMGs) and Junior Doctors working in General Practice and/or District Hospitals to support workforce requirements when there is critical risk to service continuity.
View the GP Now application from- Request for service
For Clinicians
Who we support: we support private General Practice where significant staffing challenges have occurred and an alternative solution cannot be found. The aim is to provide this service as an interim measure that bridges to a longer term sustainable and viable solution. The service works closely with the Department of Health, Primary Health Tasmania and HR+ to ensure the support provided is contributing to a plan for stable long term community healthcare.
What we do: Support is offered by Specialist General Practitioners through both virtual care and short-term physical deployment to a clinic/hospital. Additionally support to GP Registrars, IMG’s and Junior Doctors can be provided with support where safe and appropriate to do so.
Why use the service: where significant staffing challenges have occurred in a private General Practice or District Hospital and the support of a Specialist GP is as a bridge to a long-term solution.
For Consumers
Who we are: we are a group of Specialist General Practitioners across the state of Tasmania who support our colleagues in General Practice communities to deliver safe and consistent healthcare to communities.
What we do: where a General Practice or District Hospital has unexpected and significant staffing challenges we can offer support to those places. Importantly we work with organisations to make sure our support is appropriate and a part of the plan to maintain high quality community healthcare to Tasmanians.
What to expect: that where your regular General Practice is really struggling, and our service is appropriate to help that one of the GP Now doctors may be involved in your care for a short period of time.
What we can do for you: we can help ensure that you have access to continuous and safe primary care close to your home.
For more information view the Information for GPs
