Introduction
Welcome to the second edition of the Communicable Diseases Prevention Unit (CDPU) Bulletin where we provide the latest surveillance data, updates, insights, and resources relating to communicable diseases and the work of CDPU in Tasmania.
This edition provides topical communicable disease updates concerning preparedness for Highly Pathogenic Avian Influenza (HPAI), Rotavirus and Cryptosporidiosis. In addition, we provide immunisation updates related to Mpox, Shingrix, Whooping Cough (pertussis) and Respiratory Syncytial Virus (RSV). An epidemiology summary of the disease notifications in Tasmania is included.
The next edition of the Bulletin will be published in March 2025.
Annie Wells
Nursing Director, CDPU, Public Health Services
Highly Pathogenic Avian Influenza (HPAI) Preparations in Tasmania
The Department of Health (DoH) has been working closely with Department of Natural Resources and Environment (NRE) in preparation for the possible arrival of highly pathogenic avian influenza (HPAI) clade 2.3.4.4b in Tasmania.
This strain of HPAI has spread rapidly around the world in the last few years, causing widespread disease and death in birds and other animals including marine mammals.
Australia remains the only continent free of this strain of HPAI and although there have been no detections in Australia or Tasmania so far, based on what has occurred worldwide, Tasmanians should expect it to arrive, most likely via wild birds migrating from places where outbreaks continue to occur.
The risk posed by HPAI to the Tasmania public remains very low at this time.
Human infections with avian influenza are rare and require direct and close contact with infected birds or animals.
Public Health Services including CDPU has undertaken extensive preparation to be ready to manage the human health risks associated with outbreaks of HPAI in poultry, wild birds or other animals. This includes working with key stakeholders promoting seasonal influenza vaccine, developing messaging and resources on how to stay safe when dealing with sick or dead wildlife and providing advice on appropriate PPE to wear for people working with or handling sick or dead animals.
CDPU also has processes in place to assess the risk to individuals after an exposure to infected birds and animals and to monitor those who may have had a high risk exposure to HPAI and provide them with information on how to keep themselves and those around them well.
Public Health Services and the DoH Emergency Management and Response Unit (EPRU) are participating in national exercises run by Australian Government in HPAI preparedness and planning activities and have been running local scenarios to test our preparedness.
The most important message for all Tasmanians currently is if people see sick or dead birds or other wildlife, you should not touch the animals but report what they have seen to the Emergency Animal Disease Hotline as soon as possible on 1800 675 888.
Cryptosporidiosis in Tasmania
Cryptosporidiosis is a gastrointestinal infection caused by the parasite Cryptosporidium. Symptoms include watery diarrhoea and abdominal cramps and may ‘wax and wane’ for up to a month. The average incubation period is seven days but may range from one to 12 days. Risk factors for infection include contaminated water, contact with animals and contact with other infected people. Cryptosporidium oocysts (the cyst containing the parasite) can be shed in the faeces of infected people and animals. Oocysts are highly resistant to disinfectants such as chlorine and can survive in water sources such as swimming pools and spas.
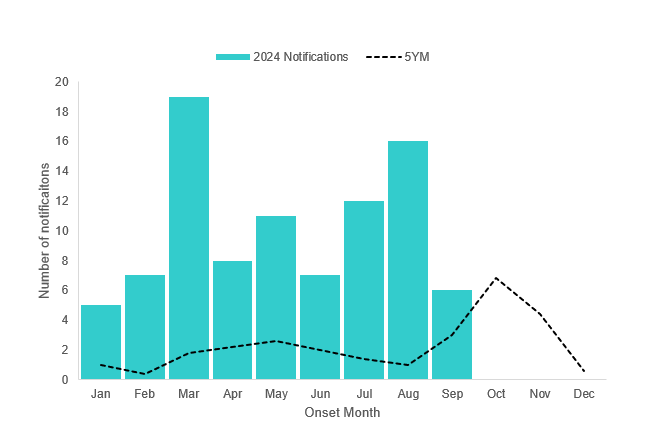
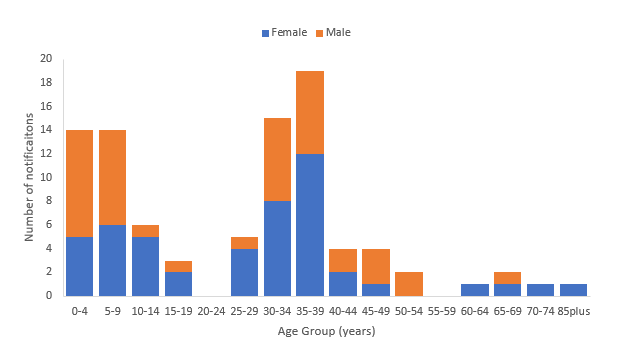
As of 30 September 2024, there have been 91 notifications of cryptosporidiosis in Tasmania this year. This is over five times more than expected compared to the five year mean of 15 notifications for the same period. The peak number of notifications occurred earlier this year in March and persisted over the autumn and winter months. Throughout 2024, monthly notifications were above expected, based on historical data (Figure 1). The median age of cases is 31 years (range 0 to 89 years) and 54% of cases are female. The highest number of notifications was in people aged 35 to 39 years (19 cases), followed by children aged nine years and under (Figure 2). The majority of cases reported this year are resident in the South (69 notifications, 76%). Other states and territories in Australia also reported high numbers of cryptosporidiosis notifications earlier this year (NNDSS Dashboard).
Through interview of cases, CDPU identified possible risk factors including interstate travel, overseas travel, swimming in a pool prior to illness onset, swimming in other water bodies (such as creeks and oceans), consumption of untreated water, contact with pets and contact with other people with a similar illness. Some cases reported more than one risk factor.
To prevent the spread of gastroenteric illnesses, including cryptosporidiosis, Public Health Services recommends keeping children home from childcare or school while unwell and for at least 24 hours after their last loose bowel motion. If you are involved in food preparation or care for others in hospitals, aged care facilities or childcare, stay home from work while unwell and for 48 hours after your last loose bowel motion. If you have Cryptosporidiosis or gastroenteritis, you should wait at least two weeks after your diarrhoea symptoms have stopped before swimming in a public pool, to prevent further spread of the parasite to other people.
More information on cryptosporidiosis can be found Cryptosporidiosis fact sheet | Tasmanian Department of Health.
Rotavirus in Tasmania
Rotavirus infection is the leading cause of viral gastroenteritis (gastro) in infants and young children globally. The most common symptoms are vomiting and diarrhoea which may lead to dehydration and severe outcomes in young children. Symptoms can take one to three days to develop and usually last one or two days. Rotavirus infection affects people of all ages, but children aged six to 24 months are at highest risk of severe disease. It is highly infectious and is spread by vomit or faeces (poo) of an infected person through person-to-person contact, contaminated objects, or contaminated food or drink. Rotavirus activity typically follows a seasonal pattern, with higher activity in mid-to-late winter.
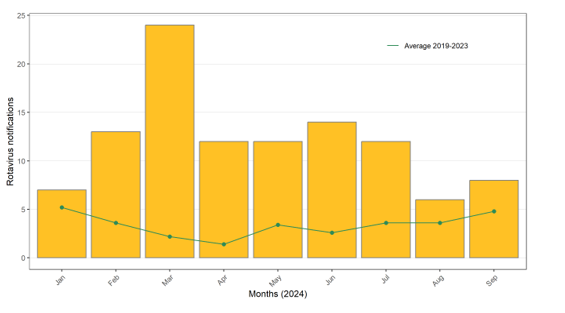
From 1 January to 30 September 2024, there were 108 notifications of rotavirus in Tasmania, compared to the 5-year average (2019-2023) of 63 notifications for the same period. Higher than average notifications were observed during all months, and the peak in notifications in March 2024 was unseasonable (Figure 1).
In line with trends observed nationally, rotavirus notifications were below baseline levels in Tasmania throughout 2020 and 2021, reflecting decreased transmission of the virus likely associated with broad public health and social measures implemented during the COVID-19 pandemic. Notifications returned to pre-COVID-19 pandemic levels in 2022. The current increase in notifications in Tasmania aligns with the increase that was reported in most other Australian jurisdictions from quarter 1 in 2023, with numbers well exceeding pre-pandemic levels.
Among cases notified this year, over half of the cases were female (59/108, 55%). Children <5 years of age (49/108, 45%) represent the age group with the highest number of notifications; of which 38% (19/108) were infants <6 months of age. Of these infants <6 months of age, 14 (14/19, 74%) had been recently vaccinated for rotavirus and had symptoms likely attributable to vaccine-related virus rather than wild-type infection.
The highest notification rate was in the South region (94 cases,1.8 per 100,000), followed by the North (8 cases, 5.1 per 100,000) and the Nort-West (8 cases, 5 per 100,00).
Handwashing with soap and running water, particularly after using the toilet, after changing nappies, and before preparing or eating food, is recommended to prevent the spread of viral gastro including rotavirus. People who are sick should stay at home and not go to work or school. Infants and children attending childcare or school should not return until at least 48 hours after the symptoms have stopped.
Vaccination for rotavirus is free for children <6 months of age. The vaccine is given as two oral doses, at two and four months of age, with completion of the course by 25 weeks of age.
Further information:
Immunisation Update
Mpox:
Mpox cases have been increasing in Australia since May 2024, and in June 2024 case numbers surpassed the previous peak in cases in August 2022. The majority of cases have been reported in Victoria and New South Wales and have been locally acquired in Australia. There have been no cases of Clade 1b in Australia yet, the clade of concern in the African region subject to a declaration of a Public Health Emergency of International Concern. The mpox vaccine JYNNEOS is available for free in Tasmania through sexual health services for at-risk and eligible individuals. JYNNEOS is not available on private script nor recommended for routine travel. See details regarding vaccine eligibility here: Mpox | Tasmanian Department of Health
Expanded Shingrix eligibility:
In November 2023, Shingrix replaced Zostavax on the National Immunisation Program (NIP) schedule. Shingrix is a non-live vaccine and is highly effective in the prevention of herpes zoster (shingles) and its complications. This has been an extremely well received program, with high demand in the community. Shingrix is funded as a two-dose schedule on the NIP for:
All adults aged 65 years and over,
Aboriginal and Torres Strait Islander people 50 years and over, and
Adults aged 18 years and older at with moderate to severe immunocompromise (expanded eligibility from 1 September 2024). To see the list of eligible immunocompromising conditions, please see the Australian Immunisation Handbook: Table. Risk conditions and immunosuppressive therapies for zoster vaccination and eligibility for NIP funding | The Australian Immunisation Handbook (health.gov.au)
Pertussis (whooping cough):
Pertussis (commonly known as whooping cough) is caused by the bacteria Bordetella pertussis. Pertussis affects people of all ages, but it can be especially serious in babies. With the increase in pertussis cases in 2024, and to protect young infants from severe illness, we are encouraging the following groups to ensure they are up to date with vaccination:
Pregnant women are recommended to be vaccinated against pertussis in every pregnancy, ideally from 20 to 32 weeks gestation. Vaccination in pregnancy provides protection to the infant in their early weeks of life while they are too young to be vaccinated.
Infants are recommended to receive their first dose of pertussis containing vaccine through the National Immunisation Program at 6 weeks of age, with subsequent doses at 4-, 6-, 18- months and 4 years of age.
Adult household contacts of infants aged <6 months are also recommended to receive vaccine at least 2 weeks before they have close contact with the infant.
Respiratory Syncytial Virus (RSV):
RSV infection can cause severe disease, particularly in very young infants and older adults. The RSV season in Tasmania typically occurs from May to September. There are two effective RSV vaccines, Abrysvo and Arexvy, currently available on private prescription in Australia. Whilst both Abrysvo and Arexvy are registered for use in adults over the age of 60, only Abrysvo is registered for use in pregnant women. Pregnant women are recommended to receive Abrysvo during pregnancy from 28weeks gestation to protect their infants against RSV in the early months of life.
The Australian Government has announced that the RSV vaccine Abrysvo will be included in the National Immunisation Program for eligible pregnant women in 2025. More details about the program start date will be available soon.
National Immunisation Program update - RSV vaccine | Australian Government Department of Health and Aged Care for more information.
Planning is currently underway concerning an infant RSV immunisation program for Tasmania ahead of winter 2025. The Tasmanian Department of Health will provide further details soon.
For more information about RSV vaccination, see the Australian Immunisation Handbook: Recommendations | Respiratory syncytial virus (RSV) | The Australian Immunisation Handbook (health.gov.au)
Notifiable Diseases in Tasmania Summary Table 1
Number of disease notifications received per quarter by onset date, Tasmania, September 2024.
| Disease Category | Disease | Quarter 1 | Quarter 2 | Quarter 3 | YTD* 2024 | YTD 2023 | YTD 2022 |
|---|---|---|---|---|---|---|---|
| Blood Borne | Hepatitis B | 17 | 12 | 14 | 43 | 34 | 48 |
| Hepatitis C | 28 | 28 | 32 | 88 | 88 | 88 | |
| Hepatitis D | 0 | 0 | 0 | 0 | 0 | 1 | |
| Enteric | Campylobacter infection | 357 | 278 | 242 | 877 | 719 | 747 |
| Cryptosporidiosis | 31 | 26 | 34 | 91 | 14 | 20 | |
| Listeriosis | 0 | 0 | 0 | 0 | 1 | 0 | |
Hepatitis A | 0 | 0 | 1 | 1 | 1 | 4 | |
Hepatitis E | 0 | 0 | 0 | 0 | 1 | 0 | |
Listeriosis | 2 | 0 | 0 | 2 | 3 | 2 | |
| Paratyphoid | 2 | 0 | 0 | 2 | 2 | 0 | |
| Salmonellosis | 105 | 65 | 38 | 208 | 200 | 153 | |
| Shiga-toxin and Vero-toxin producing Escherichia coli | 4 | 2 | 5 | 11 | 11 | 11 | |
| Shigellosis | 4 | 5 | 8 | 17 | 14 | 11 | |
| Typhoid | 0 | 1 | 0 | 1 | 4 | 1 | |
| Vibrio infection (foodborne) | 0 | 1 | 1 | 2 | 1 | 6 | |
| Yersinia | 0 | 1 | 1 | 2 | 1 | 6 | |
| Respiratory | COVID-19^ | 1,336 | 1,479 | 678 | 3,493 | 3,352 | 54,943 |
| Influenza | 232 | 805 | 2,588 | 3,625 | 3,098 | 2,870 | |
| Legionellosis | 6 | 6 | 4 | 16 | 16 | 13 | |
| Respiratory syncytial virus (RSV) | 154 | 971 | 1,327 | 2,452 | 1,782 | 3,369 | |
| Tuberculosis | 5 | 2 | 2 | 9 | 9 | 12 | |
| Sexually Transmissable Infections | Chlamydia trachomatis infection | 415 | 404 | 317 | 1,136 | 1,349 | 1,180 |
| Gonococcal infection | 84 | 95 | 87 | 266 | 285 | 201 | |
| Human Immunodeficiency Virus Infection | 4 | 2 | 2 | 8 | 6 | 11 | |
| Syphilis - Congenital | 0 | 0 | 0 | 0 | 1 | 0 | |
| Syphilis | 23 | 11 | 13 | 47 | 79 | 54 | |
| Vaccine Preventable | Diphtheria | 0 | 0 | 1 | 1 | 0 | 0 |
| Measles | 0 | 0 | 0 | 0 | 1 | 0 | |
| Meningococcal disease (invasive) | 0 | 0 | 0 | 0 | 4 | 2 | |
| Mumps | 1 | 0 | 1 | 2 | 2 | 0 | |
| Pertussis | 18 | 81 | 312 | 411 | 9 | 1 | |
| Pneumococcal disease (invasive) | 6 | 13 | 7 | 26 | 31 | 17 | |
| Rotavirus infection | 44 | 38 | 26 | 108 | 36 | 33 | |
| Varicella zoster infection (Chickenpox) | 16 | 16 | 28 | 60 | 48 | 45 | |
| Varicella zoster infection (Shingles) | 122 | 131 | 141 | 394 | 303 | 373 | |
| Varicella zoster infection (Unspecified) | 77 | 71 | 71 | 219 | 337 | 225 | |
| Vector Borne | Barmah Forest virus infection | 0 | 0 | 0 | 0 | 2 | 0 |
Chikungunya virus infection | 0 | 0 | 0 | 0 | 1 | 1 | |
| Dengue virus infection | 6 | 7 | 2 | 15 | 11 | 6 | |
| Flavivirus | 0 | 0 | 1 | 1 | 2 | 0 | |
| Malaria | 1 | 1 | 4 | 6 | 4 | 0 | |
| Rickettsial Infection | 1 | 0 | 0 | 1 | 15 | 7 | |
| Ross River virus infection | 7 | 2 | 0 | 9 | 3 | 6 | |
| Zoonotic | Hydatids | 1 | 0 | 0 | 1 | 1 | 1 |
| Leptospirosis | 1 | 0 | 0 | 1 | 0 | 1 | |
| Q Fever | 0 | 1 | 0 | 1 | 1 | 2 | |
| Other conditions | Carbapenemase-producing Enterobacterales (CPE) | 2 | 3 | 1 | 6 | 0 | 3 |
| Creutzfeldt-Jakob disease (CJD) | 1 | 1 | 0 | 2 | 1 | 1 | |
| Invasive Group A Streptococcal Disease (iGAS) | 17 | 7 | 8 | 32 | 34 | 2 | |
| Staphylococcus aureus bloodstream infection (SABSI) | 45 | 56 | 52 | 153 | 180 | 155 | |
| Vancomycin-resistant Enterococci (VRE) | 182 | 234 | 212 | 628 | 563 | 423 | |
| Vibrio infection (non-foodborne) | 8 | 3 | 0 | 11 | 2 | 9 |
Source Tasmanian Notifiable Disease Surveillance System (TNDSS).
*YTD – year to date values represent the cumulative number of notifications received from the beginning of the year until the end of the most recent reporting period/quarter.
^COVID-19 data includes confirmed cases only, as RAT registration in Tasmania ceased in 2024. For all other diseases, both confirmed and probable cases are included.
Notes on Table:
- Only notifiable conditions which had one or more case reports received during the reporting period or YTD during the previous 3 years appear in the table.
- Data are presented by period of ‘calculated onset date’ which is the earliest of true onset date if known, or the earliest of specimen collection date or notification date. For SABSI, VRE and CPE data are presented by specimen date.
- Data extracted on 16 October 2024. Information presented in this report is based on data available in the TNDSS at the time of reporting and is subject to change.
- Disease notifications are received daily from laboratories and health care providers in Tasmania.
- A detailed surveillance report on COVID-19, Influenza and RSV can be found in the RespTAS Report.
More information on the prevention and transmission of infectious diseases is available in the Infectious diseases guides and fact sheets.
Subscribe Now to receive the CDPU bulletin direct to your email.